TLDR - If you are a ketogenic lean mass hyper responder with high LDL, insist on imaging to determine your atherosclerotic risk, as this study indicates the LDL and ApoB by itself doesn't indicate a growth in plaque.
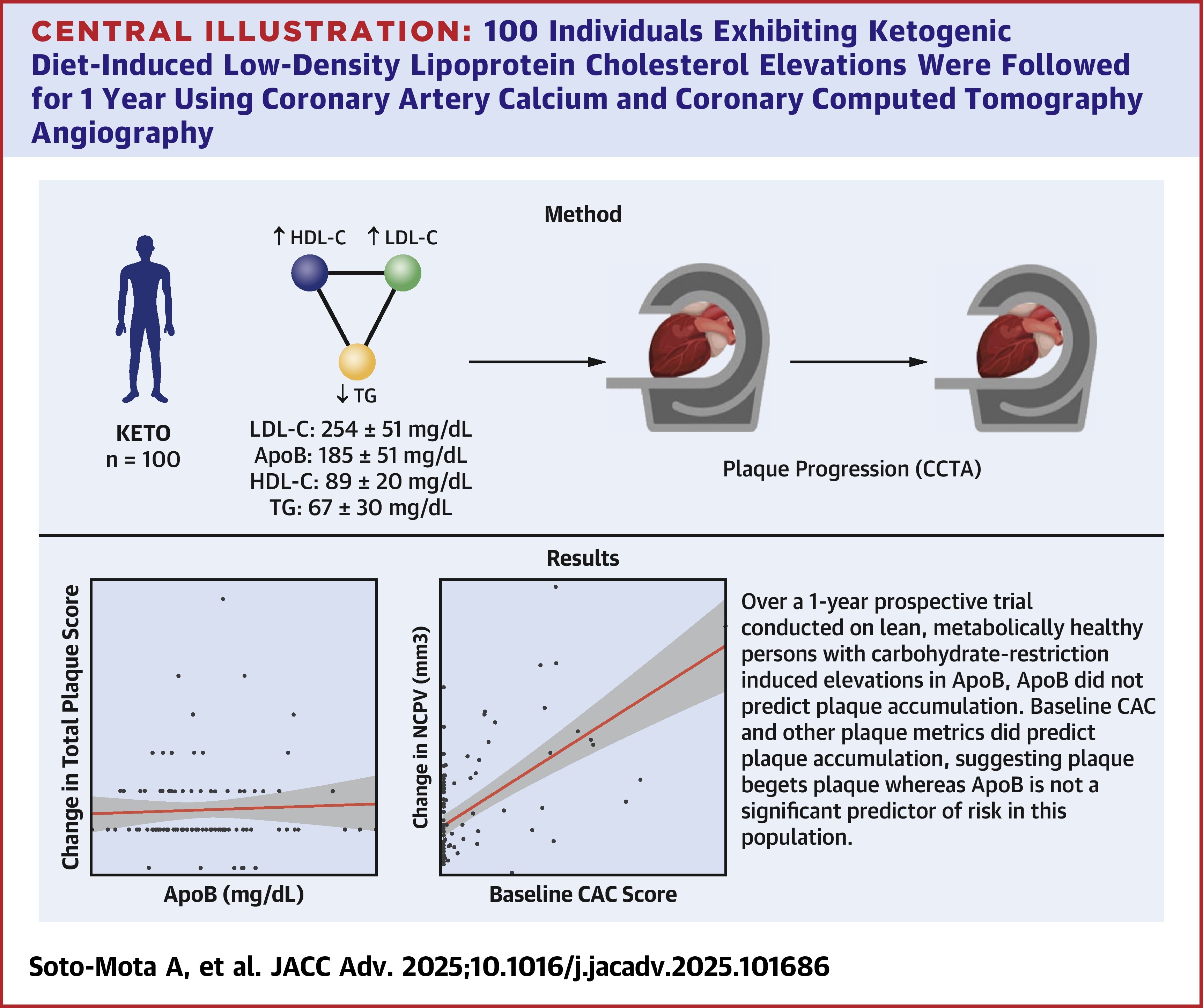
Background - Changes in low-density lipoprotein cholesterol (LDL-C) among people following a ketogenic diet (KD) are heterogeneous. Prior work has identified an inverse association between body mass index and change in LDL-C. However, the cardiovascular disease risk implications of these lipid changes remain unknown.
Objectives - The aim of the study was to examine the association between plaque progression and its predicting factors.
Methods - One hundred individuals exhibiting KD-induced LDL-C ≥190 mg/dL, high-density lipoprotein cholesterol ≥60 mg/dL, and triglycerides ≤80 mg/dL were followed for 1 year using coronary artery calcium and coronary computed tomography angiography. Plaque progression predictors were assessed with linear regression and Bayes factors. Diet adherence and baseline cardiovascular disease risk sensitivity analyses were performed.
Results - High apolipoprotein B (ApoB) (median 178 mg/dL, Q1-Q3: 149-214 mg/dL) and LDL-C (median 237 mg/dL, Q1-Q3: 202-308 mg/dL) with low total plaque score (TPS) (median 0, Q1-Q3: 0-2.25) were observed at baseline. Neither change in ApoB (median 3 mg/dL, Q1-Q3: −17 to 35), baseline ApoB, nor total LDL-C exposure (median 1,302 days, Q1-Q3: 984-1,754 days) were associated with the change in noncalcified plaque volume (NCPV) or TPS. Bayesian inference calculations were between 6 and 10 times more supportive of the null hypothesis (no association between ApoB and plaque progression) than of the alternative hypothesis. All baseline plaque metrics (coronary artery calcium, NCPV, total plaque score, and percent atheroma volume) were strongly associated with the change in NCPV.
Conclusions - In lean metabolically healthy people on KD, neither total exposure nor changes in baseline levels of ApoB and LDL-C were associated with changes in plaque. Conversely, baseline plaque was associated with plaque progression, supporting the notion that, in this population, plaque begets plaque but ApoB does not. (Diet-induced Elevations in LDL-C and Progression of Atherosclerosis [Keto-CTA]
Full Paper: https://doi.org/10.1016/j.jacadv.2025.101686
Notes from the paper:
Look at that, they verified ketone state!
For these 100 people the KD was sustainable