Friendly Carnivore
Carnivore
The ultimate, zero carb, elimination diet
Meat Heals.
We are focused on health and lifestyle while trying to eat zero carb bioavailable foods.
Keep being AWESOME
We welcome engaged, polite, and logical debates and questions of any type
Purpose
- lifestyle
- food
- Science
- problems
- Recipes
- Sustainability
- Regenerative lifestyle
Rules
- Be nice
- Stay on topic
- Don't farm rage
- Be respectful of other diets, choices, lifestyles!!!!
- No Blanket down voting - If you only come to this community to downvote its the wrong community for you
- No LLM generated posts . Don't represent machine output as your own, and don't use machines to burn human response time.
Other terms: LCHF Carnivore, Keto Carnivore, Ketogenic Carnivore, Low Carb Carnivore, Zero Carb Carnivore, Animal Based Diet, Animal Sourced Foods
Meta
If you need to block this community and the UI won't let you, go to settings -> blocks you can add it.
[Meta] Moderation Policy for Niche Communities
Carnivore Resources
YouTube Carnivore
Science Based, Factual Discussions:
Experience, testimonials:
Nutritionists/Coaches:
Lifestyle/Influencers:
Mini-Series on all aspects of the Meat science, heath, nutrition, and environment
Books Carnivore
Websites Carnivore
Excellent resource with many references on all things carnivore, may have to click around, recommend
Ketogenic Resources
Carnivore is a subset of Ketogenic eating, so all of the benefits for keto also apply here
YouTube Ketogenic
Science Based, Lectures:
Websites Ketogenic
Science, Guides, Recipes , Hard Science, highly recommended
Keto Virtual Health Program - monitoring, medication titration, coaching, excellent
Books Ketogenic
- Ketogenic : The Science of Therapeutic Carbohydrate Restriction in Human Health
- Why We Get Sick: The Hidden Epidemic at the Root of Most Chronic Disease--and How to Fight It
- How Not to Get Sick: A Cookbook and Guide to Prevent and Reverse Insulin Resistance, Lose Weight, and Fight Chronic Disease
Feel free to add any suggestions below.

- Red meat is a nutrient dense food providing important amounts of protein, essential amino acids, vitamins, and minerals that are the most common nutrient shortages in the world, including vitamin A, iron, and zinc.
- Despite claims by the World Health Organization (WHO) that eating processed meat causes colon cancer and red meat probably causes cancer, the observational data used to support the claims are weak, confounded by multiple unmeasured factors, and not supported by other types of research needed for such a conclusion. Although intervention studies are designed to test the validity of associations found in observational studies, two interventions of low-fat, low-meat diets in volunteers that failed to find a benefit on cancer were not considered in the WHO decision.
- It is likely that the association of red-meat consumption with colon cancer is explained either by an inability of epidemiology to detect such a small risk or by combinations of other factors such as greater overweight, less exercise, lower vegetable or dietary fiber intake, and perhaps other habits that differentiate those who eat the most meat from those who eat the least.
Full Paper - https://doi.org/10.1093/af/vfy009

Greg talks about his journey on the carnivore diet.
summerizer
Title: “I Didn’t Eat for 39 Hours… Then Ran 62 Miles (Fasted) — Carnivore Ultra Runner Interview”
Summary (from the video only; no sponsors, no CTAs):
• Background
- Greg describes discovering the carnivore diet via a relative (his uncle).
- Initial skepticism (“you need fiber/fruit/veg”) shifts after trying it himself.
• Pre-carnivore health/issues
- Long-standing eczema/skin problems treated repeatedly with steroid creams and pills.
- A severe rash two years prior led to more steroids; doctors framed it as “this is who you are.”
• Switching to carnivore
- Adopted a meat- and egg-based diet after conventional approaches failed.
- Within ~2 weeks he noticed significant improvement in skin/eczema.
- Reports steadier energy, reduced food preoccupation, simpler meals, and less stress about recipes.
• Training/running context
- Took up running ~1–1.5 years prior; later got into ultrarunning.
- Began experimenting with fasted training runs (dinner the night before, then run without breakfast).
• The fasted 100K (≈62 miles)
- Entered a 100-kilometer ultramarathon with a plan to remain fasted.
- Did not eat for 24 hours before the start, ate only after finishing.
- Total time without food ≈39 hours (24 hours pre-race + ~15 hours of racing).
- During the race he consumed only water and electrolytes (salt-stick type: sodium, potassium, magnesium).
- Took roughly one electrolyte capsule per hour to prevent cramps/fatigue.
- Reports no GI issues, no energy crashes, and no “hitting the wall.”
- Observed other athletes consuming large amounts of carbohydrates (he mentions ~80–100 g/hour as a common target among ultrarunners) and some experiencing bonks/crashes.
• Perceived effects/observations
- Describes stable, even energy throughout most of the race; acknowledges normal late-race fatigue but no bonk.
- Says he has “never hit the wall” since being on carnivore.
- Notes that conventional endurance advice (high-carb fueling) conflicted with his experience.
• Adaptation period & practical notes
- Warns athletes to expect an adaptation period (possibly 1–2 months of worse performance) when switching diets.
- Emphasizes electrolytes (sodium/potassium/magnesium) and hydration on carnivore/fasted runs.
- Typical pre-run approach outside of races: eat the evening meal, then run fasted the next morning.
• Social reaction & debate
- Fellow runners were surprised he attempted and completed a 100K entirely fasted.
- Mentions critics of carnivore and says he’s open to being a “guinea pig” for testing/measurement in the future.
Referenced papers (as mentioned in the video):
• None explicitly cited; no DOI-identifiable papers referenced by title or author in the conversation.
When most people tell their doctors they’ve gone carnivore, they’re met with fear, confusion, or flat-out resistance. But why? In this conversation with Dr. Tony Hampton, we break down why so many doctors are scared of carnivore, how to work within the medical system without giving up your health journey, and whether you really need your doctor’s permission to heal.
summerizer
Title: Why many doctors oppose the carnivore diet — discussion with Dr. Tony Hampton (board-certified physician & metabolic health expert)
Core question
- Why do many doctors dislike or discourage a carnivore (“proper human”) diet?
Key points from the conversation
- Medical training bias: Standard guidance emphasizes low-fat, high-carbohydrate patterns (e.g., DASH/old food pyramid with multiple daily servings of grains and fruits). When patients propose the opposite, many clinicians label it “dangerous.”
- Lipids & risk markers: Rather than focusing on total LDL alone, the discussion emphasizes:
- LDL particle characteristics (small/large particles)
- Triglyceride:HDL ratio (target: <2)
- Apolipoprotein ratios (ApoB:ApoA1) in the normal range
- Inflammatory markers (CRP, ESR) in the normal range
- Metabolic health measures: waist/belly size, blood pressure, blood sugar
- Statin default: In conventional care, elevated LDL often leads directly to a statin recommendation, without broader metabolic context.
- Fiber myth: The claim that fiber is required for bowel movements is challenged; examples given that carnivores (animals and people) have normal bowel function without fiber.
- Protein/kidney concern: Carnivore/keto are characterized as high-fat, moderate-protein (not “high-protein”). Protein is not presented as harmful to kidneys in general; adjustments may be needed for existing kidney disease.
- Evidence landscape:
- A “Harvard study” is cited as showing favorable outcomes among people following carnivore, but it was observational; more randomized controlled trials are needed for clinician confidence.
- Because carnivore is a ketogenic pattern, existing keto evidence is presented as supportive while awaiting carnivore-specific RCTs.
- Practice realities:
- Many physicians lack formal nutrition education; even proponents working inside large health systems aim to educate peers and integrate low-carb care.
- Not all patients need to be strict carnivore; many benefit from moving toward low-carb.
- Patient approach:
- Share personal results and data respectfully; request monitoring of meaningful markers.
- If a clinician is unwilling, consider finding a carnivore/low-carb-friendly doctor; patient autonomy over diet is emphasized.
- Institutions & outlook:
- Mentions professional groups (e.g., Society of Metabolic Health Practitioners) working on outreach.
- Optimism expressed about broader institutional and policy openness to metabolic-health approaches.
Referenced paper(s) with DOI
- Lennerz BS, Mey JT, Henn OH, Ludwig DS. “Behavioral Characteristics and Self-Reported Health Status among 2029 Adults Consuming a ‘Carnivore Diet’.” Current Developments in Nutrition (observational survey). https://doi.org/10.1093/cdn/nzab133
Cancer as a metabolic disease
The big fat surprise
Why we get sick
How not to get sick
Some nice physical reading ahead
You don't have to be rich to eat like Mitch
summerizer
Title: How much did I just spend for 2 WEEKS of food on CARNIVORE?
Scope: Speaker shows a Sam’s Club grocery delivery and breaks down what they’ll eat on a budget for ~2 weeks on a carnivore diet. Prices and quantities are as stated in the video.
Items & quantities
- Smoked salmon: 2 packs, 1 lb each (total 2 lb).
- Eggs (pasture-raised): 4 flats of 18 eggs (72 eggs total).
- Chicken thighs: 2 large packs (~5.2 lb each) at $7.38 per pack; “enough for at least 10 meals.”
- Hickory-smoked bacon: 4 lb total (brand mentioned as hickory-smoked/Wright-style).
- Frozen beef burger patties: 6 lb total.
- Optional add-on: a “couple of ribeyes.”
Notes on use/meals
- Salmon is paired with eggs; also called out as a quick air-fryer option.
- Burger patties are the main beef source (ribeye consumption reduced due to price).
- Bacon and eggs highlighted as a go-to meal.
- Chicken thighs planned across multiple meals (≥10).
Costs (as stated)
- Main order total (including delivery and tip): $110.
- Optional ribeyes: ~$30 for “a couple.”
- Estimated 2-week spend with ribeyes included: < $150.
Overall takeaway (from the video content)
- The speaker demonstrates a 2-week carnivore plan centered on eggs, chicken thighs, bacon, burger patties, and some smoked salmon, obtained via Sam’s Club delivery, keeping total spend around $110–$150 for the period.
Referenced papers
- None mentioned in the video.
In this thought-provoking presentation, Nina Teicholz addresses the complexities and implications of the U.S. Dietary Guidelines. She highlights how these guidelines, established in 1980, have become the gold standard for federal feeding programs and medical associations, yet are correlated with rising chronic disease rates. Teicholz critically examines the dietary recommendations, arguing that the increase in carbohydrate consumption and the decrease in intake of fats, including saturated fats, may not be supported by the latest scientific evidence. Additionally, she delves into the controversy surrounding the guidelines and the need for reform in light of conflicting research.
summerizer
Title: The Guidelines are Broken, and Always Have Been — Nina Teicholz
Scope:
- Summary strictly reflects the talk’s content as transcribed in the provided SRT. No sponsor/advertising or off-video commentary included.
Core thesis:
- U.S. Dietary Guidelines are an “incredibly powerful policy” shaping school meals, military rations, hospitals, WIC/elderly feeding, and public messaging.
- From inception, guidance (notably limits on saturated fat and total fat) rested on weak/indirect evidence and has not delivered the intended health benefits.
Historical setup & policy influence:
- 1961: American Heart Association issues first official policy recommending Ancel Keys’s idea to cut saturated fat.
- 1980 onward: U.S. Dietary Guidelines formalize low-fat, grain-heavy patterns; ripple effects worldwide.
What the Guidelines promote (as described):
- Emphasis on fruits, vegetables, grains; non-/low-fat dairy; “protein foods” increasingly from non-animal sources.
- Explicit ~10% cap on saturated fat.
- Allowed/encouraged vegetable (industrial) oils; talk specifically mentions soybean oil.
- Sugar guideline noted at ≤10% of calories.
Trends shown/claimed (from the talk’s charts and narration):
- Americans ate more of what the Guidelines told them to increase (grains, vegetable oils) and less of what they told them to reduce (red meat, eggs); poultry increased.
- Carbohydrates as a share of total calories rose; Guidelines simultaneously raised recommended carbohydrate amounts.
- Despite alignment with guidance, obesity and diabetes rose sharply over time (presented as discordant with expectations).
Evidence grading & methodological critique:
- Major clinical trials were reviewed and many did not support core low-fat/saturated-fat claims.
- Process concerns:
- Advisory committees (DGAC) allegedly avoided direct, transparent review of relevant RCTs on saturated fat and low-carbohydrate diets.
- Reliance on external/secondary reviews and computer modeling rather than prioritizing clinical trials.
- Inconsistent evidence grading; associative/observational results weighed over trials even when trials exist.
- Committee composition and conflicts of interest raised as risks to impartial evaluation.
Specific topic notes mentioned:
- Saturated fat: A 2020 “review on saturated fat” (described in the talk) is cited as emblematic of selective evaluation.
- Lipids: Total cholesterol framed as an inadequate marker; discordance between LDL-C and outcomes referenced; interest in lipoprotein subfractions implied.
- Red/processed meat: Claims of weak associative evidence with small effect sizes and heavy confounding; restrictions portrayed as poorly supported.
- Eggs/dietary cholesterol: Historical limits described as lacking robust trial support; later evidence portrayed as not confirming harm for most people.
- Refined grains: Allowances characterized as inconsistent with nutrient density and metabolic health aims.
- Sugar: The speaker argues sugar received comparatively less emphasis than fat for decades.
- Low-carbohydrate diets: Said to be under-reviewed/sidelined despite RCTs showing improvements in glycemia and cardiometabolic risk factors.
Policy stakes & international context:
- Because the Guidelines drive procurement, labeling, reimbursement, and education, misalignment with trial evidence has wide consequences.
- The talk suggests global scientists increasingly question the saturated-fat hypothesis; U.S. processes lag in updating.
Q&A highlights (end of talk):
-
Audience engagement touches on current perceptions of red meat and broader acceptance of claims despite evidentiary weaknesses.
-
Session ends shortly after a final audience exchange.
-
BMJ 2015 feature by Nina Teicholz critiquing the DGAC evidence base: https://doi.org/10.1136/bmj.h4962
This study claimed that high cholesterol on keto was safe — but did they hide the truth? I’m Dr. Eric Westman, and in this video I break down the controversial “Lean Mass Hyper-Responder” study, the accusations of buried data, and what the real science shows. After decades of clinical work with low-carb patients, I’ve seen how misinformation spreads fast, so let’s look at what actually happened here.
summerizer
Video Summary (for/against context; based solely on the video)
Context
- Format: A reaction/rebuttal in which Dr. Eric Westman plays and responds to a critical video by Mike the Vegan about a ketogenic diet coronary CT angiography (“Keto-CTA”) study.
- Core dispute: Whether the Keto-CTA study’s data and rollout support the claim that very high LDL/ApoB in lean, metabolically healthy ketogenic dieters did not predict plaque progression.
“Against” (Mike the Vegan’s critique)
- Data handling / transparency
- Accuses the authors of “gross manipulation” and burying key outcomes.
- Claims the public rollout was mishandled, including release of a figure that a senior author later said “was not the final paper.”
- Says some data had to be “squeezed” out of the authors and that this situation is unusual.
- Study framing
- Objects to calling it a “trial” or “prospective trial,” asserting it’s actually a prospective cohort and that repeated “trial” language is misrepresentative.
- Missing/underplayed outcomes
- Asks whether key CTA outcomes (e.g., percent change in non-calcified/total plaque) were “shoved under the rug.”
- Highlights mixed outcomes across participants (some progressed, some regressed) and argues the presentation overstates safety of high LDL/ApoB.
- Authorial disagreement
- Points to apparent discord among study authors and cites Dr. Budoff’s statements criticizing how a figure was released/handled.
- Call for oversight
- Urges JACC: Advances (the publishing journal) to review what went wrong and at minimum issue a correction.
“For” (Dr. Eric Westman’s rebuttal)
- Primary finding defended
- Emphasizes the study’s central observation: in lean, metabolically healthy ketogenic dieters, LDL-C/ApoB did not predict plaque progression, whereas baseline plaque burden was a strong predictor of future plaque change.
- Imaging method context
- Stresses the distinction between CTA (visualizes plaque directly, including non-calcified plaque) vs CAC (calcified plaque scoring), framing CTA as a more granular modality for this question.
- Heterogeneous outcomes are expected
- Notes it’s normal that some participants regress, some progress, and some remain stable over time; interprets this variability as consistent with real-world clinical experience.
- Study nomenclature and intent
- Treats the “Keto-CTA” label as a colloquial descriptor; focuses attention on what the imaging showed over time, not on the “trial” vs “cohort” wording dispute.
- Clinical takeaway for this population
- Reiterates the population studied (lean, metabolically healthy, long-term ketogenic dieters) and the specific result (plaque predicts plaque; LDL/ApoB didn’t in this cohort over the measured interval).
Neutral clarifications presented in the video
- Population & duration: Lean, metabolically healthy adults on long-term ketogenic diets underwent research-grade coronary CTA; follow-up imaging assessed plaque change.
- Baseline plaque matters: Existing plaque at baseline was repeatedly described as the best predictor of subsequent change.
- Outcome mix: Across individuals, progression, stability, and regression were all observed.
Papers referenced in the video (DOIs)
- KETO Trial (baseline cross-sectional CTA) — Carbohydrate Restriction-Induced Elevations in LDL-Cholesterol and Atherosclerosis: The KETO Trial (JACC: Advances, 2024).
DOI: 10.1016/j.jacadv.2024.101109 - Keto-CTA longitudinal analysis — Longitudinal Data From the KETO-CTA Study: Plaque Progression and Predictors in Lean Individuals on a Ketogenic Diet (JACC: Advances, 2025).
DOI: 10.1016/j.jacadv.2025.101686
This was a really well researched talk, surprisingly high quality.
summerizer
Title: 3 Reasons Why RFK Jr. Wants You To Eat MORE Saturated Fat
Core aims of the video
- Clarify why headlines about saturated fat often sound alarming versus what the best evidence shows.
- Keep the discussion apolitical and focused on study design and data quality.
- Offer a simple, real-food template that can include saturated fat without fear, especially for people with insulin resistance.
Why many clinicians still fear saturated fat
- The classic “diet-heart” model: saturated fat (SFA) can raise LDL; LDL is causal in atherosclerosis; therefore SFA must raise risk.
- Guidelines and medical training have reinforced this logic for decades.
- Some trials showed benefits when SFA was specifically replaced with polyunsaturated fat (PUFA), which shapes clinician perception.
What the best evidence shows (by study design)
Randomized controlled trials (RCTs)
- A rigorous Cochrane review of long-term RCTs found that reducing SFA for ≥2 years lowered combined cardiovascular events by ~17%, with little or no clear change in total mortality; benefits were greater when SFA was replaced with PUFA. DOI: 10.1002/14651858.CD011737.pub3
Observational cohorts
- The PURE study (18 countries) reported that higher total fat—including SFA—was associated with lower total mortality, while higher carbohydrate intake was associated with higher total mortality. Total fat and SFA were not significantly associated with cardiovascular disease (CVD) or myocardial infarction; SFA showed an inverse association with stroke. DOI: 10.1016/S0140-6736(17)32252-3
Broad evidence syntheses / food-based framing
- A 2020 JACC State-of-the-Art Review emphasized evaluating foods in their matrix (e.g., dairy, unprocessed meats) rather than isolating single fatty acids. It reported no benefit on CVD or total mortality from simply cutting SFA in isolation, and highlighted that food-based patterns and replacements matter. DOI: 10.1016/j.jacc.2020.05.077
How to keep the conversation apolitical
- Be precise about study designs: distinguish RCTs (causal tests) from observational studies (associations).
- Pay attention to what SFA is replaced with (PUFA vs refined starch/sugar) when interpreting results.
- Focus on clinical markers and outcomes rather than teams or headlines.
Practical eating template (especially for insulin resistance)
- Reduce refined starches and sugars.
- Within a whole-food pattern, you can include natural sources of SFA (e.g., beef, eggs, butter, cheese, full-fat yogurt) without fear when the overall metabolic context is improved.
How to track progress (not teams or headlines)
- Waist size
- Triglycerides
- HDL
- Fasting insulin
- Apo (e.g., apoB)
Bottom line from the video
- The risk story for saturated fat depends on context and replacement. RCTs suggest event reduction when SFA is lowered (especially when replaced with PUFA), large cohorts like PURE do not support harm of higher SFA within varied global diets, and modern syntheses (JACC) argue for food-based guidance rather than blanket SFA limits. The video’s practical stance: improve metabolic health first; then saturated fat from whole foods can fit.
Back in 2011, Denmark passed a law taxing foods high in saturated fat. The tax was apparently effective in reducing saturated fat intake among Danish consumers, which reportedly dropped by about 4% during the time it was in place.
That's intense
TLDR Summary
- There is no convincing evidence that replacing saturated fat with PUFA reduces risk.
- Saturated fat is found in many healthy foods
This article builds on https://www.dietdoctor.com/researchers-challenge-who-draft-recommendations-on-saturated-fat-restriction
Which brings up these points
- Foods containing saturated fats are very diverse
- Unconvincing evidence that reducing saturated fat decreases heart disease risk
- Reliance on LDL cholesterol values to determine risk
- Many nutritious foods are high in saturated fat
TLDR for the TLDR - Chasing lower LDL numbers does not translate into better health in isolation.
Professor Noakes has published more than 750 scientific books and articles. He has been cited more than 16 000 times in scientific literature, has an H-index of 74 and is rated an A1 scientist by the National Research Foundation of South Africa. After coming across research which denounced current international dietary guidelines as fallacy, Prof Noakes started researching the effects of carbohydrates, proteins and fats on the human race. His research convinced him that a high fat, low carb diet is the healthiest option for many. After being left frustrated by a decline in his personal health, Prof Noakes has made it his mission to reverse the global trend and redefine the dietary guidelines. The Noakes Foundation is the catalyst for this change. It seeks to reveal what genuine healthy nutrition looks like and, in doing so, make a difference in the lives of millions of people.
summerizer
Title: How Do We Really Fuel Athletic Performance? — Dr. Shawn Baker & Prof. Tim Noakes
Participants
- Host: Dr. Shawn Baker
- Guest: Prof. Tim Noakes
Core Thesis
- The prevailing narrative that high-carbohydrate intake is essential for peak athletic performance is overstated. Human performance can be supported—and in many cases improved—by relying more on fat oxidation, with carbohydrate needs being lower than commonly promoted.
Key Points
Metabolic Priorities & Fuel Use
- Muscles preferentially burn carbohydrate when insulin is elevated; high-carb eating keeps insulin high and suppresses fat oxidation.
- At rest, using “jet fuel” (carbohydrate) makes little sense metabolically; fat should be the dominant fuel outside of high-intensity bursts.
- Muscle glycogen appears to act more as a regulator/signal of carbohydrate oxidation rather than a strictly limiting fuel during most efforts.
Glycogen: Role, Misconceptions, and Evidence
- Classic glycogen-loading concepts have been overemphasized; performance does not track linearly with “topping up” muscle glycogen.
- Studies cited from the 1990s: subjects with high muscle glycogen at rest still preferentially burned carbohydrate due to hormonal signaling (insulin), not because glycogen was limiting.
- Infusion experiments (described) suggest carbohydrate burning can be driven by carbohydrate availability/insulin rather than necessity.
Hypoglycemia & Performance
- Performance drops are linked to falling blood glucose during exercise; athletes often interpret this as “needing more carbs,” yet the underlying issue is metabolic inflexibility driven by chronically high-carb intake.
- Training/lifestyle that improve fat oxidation reduce susceptibility to exercise-associated hypoglycemia.
Carbohydrate–Insulin Model & Metabolic Health
- A high-carb pattern (especially frequent feeding) elevates insulin chronically, promoting carbohydrate dependence and insulin resistance over time.
- Many modern athletes show signs of insulin resistance despite high training volumes; shifting to lower-carb patterns can improve metabolic health and fuel flexibility.
Low-Carb / Fat-Adaptation in Sport
- Fat adaptation (weeks to months) increases the body’s capacity to oxidize fat at given workloads, decreasing reliance on frequent carbohydrate dosing.
- For submaximal endurance intensities, fat provides ample energy; carbohydrate needs cluster around higher-intensity efforts.
- Practical takeaway: prioritize fat-based fueling for most training/competition, with situational carbohydrates for decisive high-intensity segments if needed.
Hydration, Sodium, and “Electrolyte” Messaging
- Sweat sodium loss is often overstated; the body adapts by conserving sodium with reduced sweat sodium over time.
- Hyponatremia risk is driven more by overconsumption of fluids and excess sodium intake patterns than by sweat losses alone.
- The sports drink/electrolyte narrative has commercially amplified sodium and carbohydrate needs beyond what physiology requires for most athletes.
Elite Performance Context
- Success of East African runners is tied to lifelong habits, body composition, altitude exposure, and training culture—not to high supplemental carbohydrate regimens per se.
- Training quality and metabolic health trump aggressive carb-loading in explaining elite outcomes.
Aging, Training, and Monitoring
- Maintaining performance with age is feasible via consistent training, strength preservation, and metabolic health.
- Personal monitoring (glucose, insulin context, performance metrics) can guide individualized fueling rather than defaulting to high-carb prescriptions.
Industry Influence & Narratives
- Historical sports science was influenced by commercial interests (carb drinks/“electrolytes”), shaping guidelines that overprescribed carbohydrate and sodium.
- Re-examining these narratives with physiology-first reasoning suggests lower carbohydrate requirements and more reliance on fat for most athletic work.
Actionable Summary
- Train the ability to burn fat (dietary pattern + aerobic base).
- Use carbs tactically for high-intensity efforts rather than continuously.
- Avoid overdrinking and unnecessary sodium loading; let thirst and adaptation guide.
- Track personal responses (energy, glucose trends, performance) to fine-tune fueling.
In this episode, Dave sits down with Peter Ballerstedt, a retired forage agronomist and ruminant nutritionist known as "Don Pedro the Sod Father of the Ruminati," who brings a unique agricultural perspective to metabolic health discussions. Ballerstedt shares his 2007 transformation after reading Gary Taubes' book and how it led him to bridge agricultural science with the low-carb community. The conversation examines environmental arguments around animal agriculture, presents data on greenhouse gas emissions (12% animal vs 10% plant agriculture), explores the limitations of converting grassland to cropland, discusses the evolution of dietary guidelines since the 1970s, and examines Ballerstedt's concept of a "ruminant revolution" to address both human malnutrition and environmental concerns.
summerizer
Summary: “The Hidden Truth about Cows and Climate Change – TFP #010 | Peter Ballerstedt, PhD”
Context & Guest
- Guest: Peter Ballerstedt, PhD (forage agronomist; background in grazing systems, forage science, and ruminant agriculture).
- Focus: Ruminant agriculture’s role in nutrition, ecology, and climate; protein quality; land use; soil and carbon dynamics; common misconceptions about cattle and climate.
Key Themes
-
Ruminants & Human Nutrition
- Animal-source foods supply essential, highly bioavailable nutrients that are sparse or poorly available in staple cereals.
- Cereals dominate global protein tonnage but are poor-quality protein sources compared with animal-source foods.
- Crude protein estimates from plant foods can be inflated by non–amino-acid nitrogen (e.g., nitrate), overstating true protein content available to humans.
- Protein “quality” matters in addition to quantity; differences in amino acid patterns and digestibility change the effective nutrition delivered.
-
Land Use & “Marginal” Lands
- Large areas used by agriculture are non-arable or “marginal” (e.g., steep slopes, thin soils, altitude, drought/low rainfall) and not suitable for tillage/cropping.
- Ruminants convert forages grown on such lands—inedible to humans—into nutrient-dense food, enabling food production without competing for prime cropland.
-
Grazing, Soils, and Ecosystem Services
- Well-managed grazing can improve ground cover, root mass, water infiltration, and soil structure.
- Manure and urine return nutrients to soils; ruminant–forage systems participate in nutrient cycling.
- Pasture systems differ from annual tillage-based systems in disturbance patterns and can help maintain or improve soil function when managed appropriately.
-
Carbon & Methane Framing
- Emissions discussion often conflates short-lived methane with long-lived CO₂.
- The timescales and biogenic cycling of methane differ from fossil CO₂; the framing used affects perceived impact.
- Modeled long-range climate projections carry lower confidence than immediate, observed conditions; choice of model and assumptions drives conclusions.
-
Dietary Shifts vs System-Level Levers
- Recently discussed assessments (e.g., from global bodies) indicate that voluntary personal dietary change is among the least impactful strategies for achieving sectoral emissions targets in animal agriculture compared with other system-level interventions.
- Proposals to “remove animal products” imply replacing them with plant products that must match the nutrient delivery—this is a small set of options with practical agronomic constraints (where and how those replacements would be grown).
-
Historical Nutrition Narratives
- Greenland Inuit/Eskimo “paradox” is referenced: early observations of low heart disease despite a high-fat diet led to a fish-oil–centric explanation; however, much of the fat intake was from mammals, not fish.
- Takeaway presented: long-standing narratives about dietary fat sources and cardiovascular risk were shaped by selective interpretation of early observations.
-
Forage Agronomy Basics (Explained Accessibly)
- Forage crops: plants (grasses/legumes/forbs) grown to be eaten by ruminants; distinct from seed/grain crops.
- Feed analysis pitfalls: nitrogen-based crude protein vs true amino-acid content; implications for ration formulation and human-food analogies.
-
Systems Thinking & Trade-offs
- Agriculture is multi-dimensional: nutrition, ecology, economics, and culture intersect.
- Policies should consider definitions/denominators used in metrics; changing denominators or category buckets can invert conclusions.
Specific Points & Examples
- Animal-source foods deliver nutrients (vitamins, minerals, essential amino acids) in forms and densities difficult to match with cereals alone.
- Wheat noted as a large global protein contributor by mass but a “poor” protein source in quality terms.
- Soil health and productivity depend on management; grazing practices can be net beneficial in many contexts when tailored to local conditions.
- Large shares of agricultural land unsuitable for crops can still produce food via ruminants, avoiding direct competition with cropland.
Practical Implications Stated in the Video
- Eliminating ruminants would require credible, agronomically feasible plant replacements capable of delivering equivalent nutrients at scale.
- When evaluating climate strategies in livestock, prioritize high-yield levers over low-impact voluntary diet shifts if the goal is measurable sectoral reductions.
- Interpret claims about livestock emissions with appropriate understanding of methane’s biogenic cycle vs fossil carbon’s accumulation.
Bioengineering professor Annelise Baron reveals why carnivore works so effectively and how to turn off disease.
https://bioengineering.stanford.edu/people/annelise-barron
Dr. Barron is a chemical and biological engineer with a keen interest in systems-level analyses of the mechanisms of complex human diseases. She was trained in chemical engineering at the University of Washington (B.S., 1990) and U.C. Berkeley (Ph.D., 1995, mentored by Prof. Harvey W. Blanch), and was a Pharmaceutical Chemistry postdoc with Prof. Ken A. Dill (UCSF) and Dr. Ronald N. Zuckermann (Chiron Corp.). She has served on the faculty at Stanford since 2007, and prior to that, worked on the Chemical & Biological Engineering faculty of Northwestern University in Evanston, IL for 10 years (1997-2007). Dr. Barron has been awarded the NIH Pioneer Award via the NIH National Institute on Aging (2020), the Oskar Fischer Award (2022), the Presidential Early Career Award for Scientists & Engineers (PECASE) through NIH / NHGRI (1999), the Beckman Young Investigator Award (1999), and the Camille Dreyfus Teacher-Scholar Award (1998), among other awards. Dr. Barron was the youngest scientist ever to serve on the Scientific Advisory Committee to the Director of the NIH, under Dr. Elias Zerhouni. She has more than 177 publications and a current H-index of 58 (Web of Science, All Databases, Barron Annelise E), and is a co-founder and serves on the advisory boards of 5 different biotechnology companies. She is proud to be 1/4 Quechua (the Native American people of Bolivia), 1/4 Spanish, 1/4 Swedish, 1/4 English, and 100% American.
summerizer
Title: Bioengineering Professor Reveals How Carnivore “Turns Off” Disease
Participants
- Host: Dave
- Guest: Prof. Anelise (bioengineering), age 56
Guest Background & Starting Point
- Lifelong academic/research background in bioengineering.
- Long history of health problems including severe psoriasis, chronic inflammation, pain, metabolic symptoms, and dental/gum issues.
- Previously tried standard dietary advice with poor results.
How She Found Carnivore
- Discovered carnivore through online interviews and community anecdotes.
- Began a strict elimination approach: primarily beef, eggs; water and salt. Removed sugars, refined carbohydrates, and most plant foods.
Personal Results Reported
- Rapid and sustained remission of psoriasis and chronic inflammation.
- Marked reductions in pain and overall symptom burden.
- Improved metabolic markers and body composition (described qualitatively).
- Better dental/gum health and fewer oral issues.
- Increased emotional stability and stress tolerance.
- Benefits strengthened with tighter adherence (fewer carbohydrates/plant foods).
Core Mechanistic Claims (as stated in the video)
- Sugar/High Glucose → Suppresses innate antiviral defenses.
- High-glucose environments can downregulate cellular antiviral programs; removing dietary sugar helps “turn them back on.”
- Hidden Lab Artifact: High-Glucose Media
- Many in-vitro studies use high-glucose culture media, potentially masking innate antiviral/immune behaviors that appear under low/no-glucose conditions.
- Viral Triggers & Chronic Disease
- Many chronic diseases have infectious/viral components (e.g., herpesviruses, Epstein–Barr virus).
- When innate antiviral immunity is suppressed (e.g., by high sugar), latent/chronic infections can drive pathology (brain, nerves, gut, skin).
- Oral Pathogens & Systemic Disease
- Gum disease/bleeding gums and pathogens (e.g., gingivalis) are linked with orodigestive cancers and neurodegeneration.
- Improved oral health reported after dietary change; posited to reduce systemic inflammatory/oncogenic burden.
- Cancer & Metabolism
- Tumor cells favor glycolysis; restricting sugar/carbs shifts cellular energetics and may disadvantage pathogens/tumor processes.
- Innate Immune Sensors
- Pattern-recognition pathways (e.g., TLRs; “receptor 9” mentioned) may behave differently under low-glucose states, revealing immune functions not seen in high-glucose conditions.
Dietary Pattern & Practical Notes
- Baseline: ruminant meat (beef emphasized), eggs; water and salt.
- Optional: small additions like cheese/butter were mentioned, but stricter carnivore produced stronger benefits.
- Carbohydrate reintroductions (including honey/sweets) were associated with symptom return.
- Fasting is discussed as synergistic with carnivore for immune/metabolic reset.
Conditions & Case Mentions (from discussion)
- Psoriasis: cleared substantially on strict carnivore.
- Metabolic issues (diabetes risk, weight): improved with carbohydrate restriction.
- Neuro/immune themes: multiple sclerosis, neurodegeneration, and chronic viral hypotheses discussed in the framework of antiviral immunity and sugar restriction.
- Orodigestive cancers: linked conceptually to oral pathogens and diet.
Implementation Philosophy
- Treat carnivore as a therapeutic elimination diet to identify triggers.
- Prioritize nutrient-dense animal foods; minimize sugars/refined carbs/plant irritants.
- Use strict adherence to test causality; loosen only after stable remission.
- Monitor oral health as a window into systemic inflammation/infection.
Open Questions & Research Directions (as posed in the video)
- How much do high-glucose lab conditions distort immunology results?
- Which diseases are most responsive to carbohydrate restriction via antiviral/immune pathways?
- What is the dose-response between small carb reintroductions and symptom recurrence?
- Can controlled trials validate the proposed sugar-immunity-infection axis across dermatologic, neurologic, and oncologic conditions?
Takeaways (as presented)
- Removing sugars/refined carbs and adopting a strict carnivore template can “turn on” antiviral defenses and “turn off” chronic disease processes for some individuals.
- Symptom improvements (skin, pain, metabolic, oral health) are closely tied to adherence and carbohydrate avoidance.
- The guest frames carnivore/very-low-carb nutrition as an immune/metabolic therapy rather than merely a weight-loss diet.
Dr. Georgia Ede and Dr. Bret Scher discuss the recently released EAT-Lancet diet report.
I found it particularly interesting that they responded to the criticism of the first report by re-releasing it and removing the parts of the report that were criticised, without directly addressing the criticism.
Dr. Sher:
In advance of the release of the 2.0 [diet report], there was actually a release of the "mis-influencers" who have done an organized approach to discredit and attack EAT-Lancet. Their words, not mine. And you were listed as a very high-ranking member of this. So first, how does it feel to be labeled as a "misinfluencer"?
Dr. Ede:
It's interesting. I actually think it's a very good thing. And the reason why is clearly [that] the content that I produced that criticized the EAT-Lancet report came to their attention. I think that that's no small thing, and I would like to believe that the content that I and others produced had a lot to do with the fact that they felt the need to produce this report to try to discredit all of us. I think it may also have had something to do with the way the report was re-released. I noticed that certain things that I criticized about the report are no longer there, and I'm not the only one who produced content critiquing the report.
Also, there are certain concerns that I and others voiced about the content of the report, and it appears as though the authors have gone to great lengths to try to acknowledge and address [these concerns] without actually addressing them. But they're trying to make it look as though they're addressing these shortcomings.
Summary
Title: Exposing the Truth Behind EAT-Lancet’s Diet Report & MisInfluencer Campaign
- The EAT-Lancet report aims to control global dietary habits by promoting a plant-based diet for planetary health, but its scientific foundation is questioned.
- The report's dietary recommendations are criticized for being nutritionally inadequate, particularly for vulnerable groups like pregnant women, children, and the elderly.
- The EAT-Lancet diet is accused of disregarding the nutritional benefits of animal-based foods, which are essential for optimal human health, including brain development and mental health.
- The report heavily relies on nutrition epidemiology, which is considered unreliable for making global dietary recommendations.
- The EAT-Lancet diet is criticized for being overly restrictive and not accounting for individual differences in metabolism, genetics, and cultural food preferences.
- The report's authors are accused of having conflicts of interest, as they are connected to major food corporations that produce ultra-processed foods and chemical fertilizers.
- The EAT-Lancet diet is seen as an attempt to control people's eating habits, rather than promoting a flexible and inclusive approach to nutrition.
- The report's dietary recommendations are criticized for being based on untested theories and guesswork, rather than solid scientific evidence.
- The EAT-Lancet diet is accused of being environmentally unfriendly, as it does not adequately address the environmental impact of industrial plant food production.
- The report's authors are criticized for labeling critics as 'mis-influencers' without providing substantial evidence to support their claims.
Loved the pictures of all the breeds of cow and also the description of how they've come about and what they taste like. I personally don't actually like A5 Wagyu that much, but plain old Japanese beef and not Wagyu I like a lot.
The colour of the fat showing how nutritious it is (yellow = grass fed) is a nice bit of knowledge to have! I'd also love to be able to dry age my own beef, but I think that's quite an endeavour. Would make a nice project to do on the side, maybe.
::: spoiler Results

Why are so many people suddenly walking away from the carnivore diet? Sarah Franklin and I break down the truth behind the trend.
If you’ve ever felt confused or frustrated about “doing carnivore the right way,” this episode will give you some clarity.
TLDW: This is the insulin stimulation issue we have discussed before. Eating enough protein at one time to stimulate enough insulin periodically is the key.
summerizer
Title: "Why is everyone QUITTING CARNIVORE?!"
Participants:
- Host Courtney Luna
- Sarah Franklin — nutritionist, 7 years carnivore; prior work in pharmaceutical industry with training in diabetes/cardiology at the International Diabetes Center.
Core Question:
- Are people quitting because “carnivore is the problem,” or because of unresolved root causes and common implementation mistakes?
Key Points From Sarah Franklin:
- Many who “feel better adding carbs back” may be masking unresolved issues rather than fixing root causes.
- Frequent pattern observed: undereating protein despite being on a meat-based diet; ramping up protein capacity often takes time.
- Early keto messaging overemphasized fat; chronically low insulin (from very low glucose exposure) can paradoxically keep blood sugar higher since insulin’s job is to lower blood glucose.
- The body can derive glucose from meat via gluconeogenesis; therefore, “needing carbs” is not a given.
- Fasting is often misapplied: some who struggle on carnivore are actually over-fasting (or still fasting) and then blaming carnivore.
- Meal timing matters: eating earlier aligns with higher insulin sensitivity and circadian rhythms; long late-day fasting windows may work against hormones.
- Hydration & electrolytes: carbs retain water; adding carbs can make people feel better quickly due to hydration and electrolytes rather than carbohydrate necessity. More protein intake requires more water; inadequate electrolytes/water can drive symptoms.
- Fat leanness: staying “super-lean” or consistently choosing very lean cuts can cause issues; appropriate dietary fat is part of making carnivore sustainable.
- Fructose consideration: even without a blood glucose spike, fructose can drive visceral fat (liver-directed metabolism); lack of a glucose spike ≠ lack of harm.
- Biomarkers can mislead:
- Blood work (glucose/ketones) is variable across the day.
- HbA1c may appear higher in some carnivores potentially due to red blood cell longevity (mentioned as a possibility; not presented as certain).
- Emphasis on assessing visceral fat/internal health rather than only labs.
- Symptom-led troubleshooting over diet-label changes:
- Examine what and when you’re eating, total protein, fat level, hydration/electrolytes.
- Consider stress, sleep, and broader endocrine context (adrenals, thyroid, sex hormones) — blood sugar regulation is upstream in the cascade.
- Digestive support/gut issues and individualized adjustments may be needed.
- “Feeling better” after carb reintroduction does not necessarily mean carbs are the solution; could reflect hydration/electrolyte changes or temporary relief rather than addressing the root problem.
Named Individuals/References (as discussed in-video):
- Mentions of community figures and perspectives, including:
- Nutrition with Judy (Judy Cho)
- Dr. Paul Saladino (noted early views)
- Dr. Sean O’Mara (visceral fat focus)
- No specific scientific papers or DOIs are cited in the discussion.
Actionable Themes (as stated by the guest):
- Prioritize adequate protein and appropriate fat.
- Avoid misapplied or excessive fasting while blaming the diet.
- Align meal timing with circadian insulin sensitivity (earlier eating).
- Ensure hydration/electrolytes scale with protein intake.
- Focus on visceral fat and internal health, not just fluctuating lab numbers.
- Address root causes (stress, sleep, hormones, digestion) rather than switching diets at the first sign of discomfort.
Today we talked heavily on ketogenic diet, creatine, brain trauma, sporting performance, the processed foods industry, suppression of voices and even Boeing airlines
Ok, this isn't the normal science focused podcast, it's a bunch of lads riffing with Chaffee acting as the content referee, but they do go into the bad science, as well as the normal mitochondria and autophogy mechanisms.
The 49:00 mark is when they go into the bad science.
summerizer
Video Summary — “#243 - Dr Anthony Chaffee - Carnivore King - Ketogenic Diet”
Who/Context
- Guest: Dr. Anthony Chaffee (physician known for advocating carnivore/ketogenic diets).
- Format: Long-form conversation focused on physiology, metabolism, and practicalities of a meat-based ketogenic diet.
Core Claims & Rationale
- Carnivore/Ketogenic basics: Emphasizes meat, eggs, and animal fats; very low carbohydrate intake to maintain nutritional ketosis.
- Metabolic framing: Argues many chronic conditions are driven by hyperinsulinemia and metabolic dysfunction; ketogenic/carnivore approaches aim to lower insulin, stabilize glucose, and reduce systemic inflammation.
- Plant defense chemicals: Asserts that plants contain bioactive compounds (toxins/antinutrients) that can irritate the gut or immune system in susceptible people; contrasts this with animal foods as “species-appropriate” and nutrient-dense.
- Mitochondria & cancer metabolism: Highlights the idea that cancer is fundamentally a metabolic/mitochondrial disease (Warburg hypothesis), discussing aerobic glycolysis (“Warburg effect”) and experiments suggesting mitochondrial health influences malignant behavior.
- Epidemiology vs interventions: Critiques observational nutrition studies (e.g., large cohort questionnaire studies) for confounding/recall bias; stresses preference for randomized/interventional evidence and mechanistic plausibility.
- Seed oils & processed foods: Recommends avoiding industrially processed foods and seed oils; favors ruminant fats/tallow and minimally processed animal foods.
Health Topics Discussed
- Weight & metabolic health: Reports frequent observations of fat loss, improved glycemic control, and satiety on ketogenic/carnivore diets.
- Autoimmune & GI issues: Discusses anecdotal/clinical observations of symptom improvements (e.g., IBD/Crohn’s) when eliminating trigger foods and carbohydrates.
- Lipids: Notes that LDL responses can vary; places greater emphasis on triglycerides, HDL, insulin sensitivity, and inflammatory markers within a broader metabolic context.
- Neurologic/brain energy: Mentions ketones as an efficient brain fuel; touches on autophagy and mitochondrial support when carbohydrate restriction reduces insulin/mTOR signaling.
- Athletics & performance: Shares examples/anecdotes of endurance performance on low-carb/carnivore approaches once adapted.
Practical Guidance Mentioned
- Transition/adaptation: Expect a 2–4 week adaptation (“keto-adaptation”); prioritize electrolytes (salt) and adequate dietary fat to avoid low-energy symptoms.
- Food choices: Center meals on ruminant meats (beef/lamb), eggs, and animal fats; keep carbohydrates minimal.
- Satiety & meal frequency: Eat to satiety; many naturally drift toward fewer meals without forcing fasting.
- Lifestyle add-ons: Sleep, stress management, and sunlight/time outdoors are encouraged as supportive factors.
Common Objections Addressed
- “Red meat & cancer/heart disease” headlines: Attributes much of the fear to observational studies and confounding; argues mechanistic/clinical data don’t support blanket restrictions for everyone.
- “Fiber is essential” claim: Suggests fiber is not universally required and can be problematic for some individuals with GI issues; emphasizes individualized responses.
Referenced Papers (with DOI)
- Otto Warburg — “On the Origin of Cancer Cells” (1956, Science) — foundational paper proposing a metabolic/mitochondrial basis of cancer.
DOI: 10.1126/science.123.3191.309
I took on one of Seoul’s most famous street food markets — Myeongdong — but with a twist: no sugar, no carbs… only meat. 🍢🔥
While everyone else was diving into sweet treats and fried carbs, I hunted down every protein-packed option I could find. From sizzling skewers to hidden carnivore-friendly stalls, this was not your typical food tour.
How hard is it to stay carnivore in the carb capital of Seoul?
The carnivore page on Wikipedia is very opinionated against carnivore. If you look at the talk section, you can see the debate, it's currently considered a pseudoscientific field, and the inclusion criteria for paper is is quite high. The editors s definitely are not open to carnivore, and that's okay, but they are the editors of the carnivore page, so they should at least be objective. They should apply the same med RS rigor to the downside of carnivore that they do to the upsides.
To that end... I've been playing around with a LLM to generate a updated version of the Wikipedia page strictly following the Wikipedia MedRS guidelines.
generated carnivore health section
Health Effects of the Carnivore Diet
Evidence disclaimer: There are no long-term clinical trials evaluating the health effects of a carnivore diet (a diet consisting exclusively of animal-source foods, eliminating all plant foods, and being very low in carbohydrates). All medical claims about this diet—positive or negative—are based on indirect evidence from other dietary contexts, including:
- Low-carbohydrate and ketogenic diet trials (not carnivore; include plant foods and refined vegetable oils)
- Observational red and processed meat studies in mixed Western diets (not ketogenic; confounded by refined carbohydrates and vegetable oils)
- Anecdotal reports (not clinical evidence)
Because no carnivore-specific randomized trials or prospective long-term studies exist, the long-term safety and efficacy of the carnivore diet are unknown.
Metabolic Context Matters
Most studies used to evaluate carnivore come from metabolic environments different from those induced by carnivore eating. Metabolism functions differently depending on fuel source:
| Feature | Carbohydrate-based metabolism | Ketogenic metabolism |
|---|---|---|
| Primary fuel | Glucose | Fatty acids and ketones |
| Insulin levels | Moderate–high | Low |
| Triglycerides | Often higher | Often lower |
| LDL behavior | Less variable | Highly variable by individual |
| Fuel regulation | Glycolysis dominant | Fat oxidation dominant |
| Gut environment | Dietary fiber present | Zero-fiber |
These represent general tendencies; individual responses vary.
Since carnivore induces nutritional ketosis, findings from carb-based diets cannot be directly transferred. Even ketogenic diet trials do not fully apply to carnivore because they include plant foods, fiber, and plant oils. Metabolic context limits evidence transfer.
Overview of the Carnivore Diet
The carnivore diet consists of meat, fish, eggs, and sometimes dairy. Compared to standard ketogenic diets, a carnivore diet:
- Is very low in carbohydrates
- Is higher in animal protein and saturated fat
- Excludes plant-derived fats (olive oil, nuts, seeds)
- Creates a fiber-free dietary pattern
Supporters claim reduced inflammation, improved metabolic health, higher energy, and autoimmune relief. Critics warn of LDL elevation, nutrient deficiencies, cancer risk, and long-term organ stress. None of these claims are supported by carnivore-specific clinical trials.
Metabolic Effects (Glucose, Insulin, Weight)
Indirect evidence suggests carbohydrate restriction can improve metabolic markers:
Interpretation: Short-term metabolic improvements are plausible under carbohydrate restriction. However:
- No studies isolate exclusive animal-based diets
- Long-term safety is unknown
- Biomarkers ≠ clinical outcomes
LDL Cholesterol and Cardiovascular Markers
LDL cholesterol often increases in a subset of individuals using ketogenic diets:
LDL is a causal factor in atherosclerotic cardiovascular disease (ASCVD) in general populations:
(Ference et al., 2017, The Lancet – genetic evidence confirming LDL causality in ASCVD)
(Silverman et al., 2016, Circulation – CTT Collaboration; lowering LDL reduces cardiovascular events)
However, no randomized trials of ketogenic or carnivore diets have reported major adverse cardiovascular events or mortality, so it is unknown whether LDL changes in a fat-based metabolic state carry the same risk.
Heart Disease Claims
Epidemiologic studies often cited against carnivore do not study ketogenic or meat-only diets:
Heart disease risk on carnivore remains unstudied.
Cancer Claims
Cancer claims rely on observational association—not causation:
These findings cannot be transferred to a zero-carbohydrate, all-meat diet without direct evidence.
Gout and Uric Acid
Gout concerns rely on general population purine studies:
Gout incidence on carnivore is unknown.
Kidney Function
There are no systematic reviews or clinical trials examining renal function on exclusive animal-source diets. Safety and harm claims are unproven.
Nutrient Adequacy
Deficiency claims rely on general nutrition guidelines, not carnivore data:
(World Health Organization – Healthy Diet guidance; mixed-diet assumptions; not carnivore-specific)
(European Food Safety Authority, 2017 – Dietary Reference Values; population nutrient estimates; not meat-only physiology)
No study has measured micronutrient blood status on a carnivore diet.
Gut Microbiome
Microbiome arguments are speculative because zero-fiber diets have not been studied clinically:
Microbiome effects on carnivore are unknown.
Autoimmune and Neurological Claims
Reports of symptom improvement for autoimmune and psychiatric conditions are anecdotal only. No controlled trials assess carnivore for these conditions.
Safety in Specific Populations
There is no safety research for:
- Children and adolescents
- Pregnant or breastfeeding women
- People with kidney or liver disease
- Long-term elderly use
Final Assessment
| Area | Evidence Status |
|---|---|
| Short-term metabolic effects | Plausible; unproven for carnivore |
| LDL effects | Increases occur in subset; clinical significance unclear |
| Cardiovascular outcomes | No event or mortality trials |
| Cancer risk | Unknown |
| Kidney outcomes | Unknown |
| Nutrient status | Unknown |
| Microbiome | Unknown |
| Autoimmune/neurological | Anecdotal only |
| Pediatric/prenatal safety | Unknown |
Conclusion: Current evidence is insufficient to declare the carnivore diet safe or harmful long-term. Most claims rely on indirect evidence from non-carnivore metabolic contexts. Carnivore-specific randomized trials are required to reach evidence-based conclusions.
I found this really pleasant to listen to so I thought I'd share. It's nice to hear someone talk about the fat loss, satiety, and all the other things that I also experienced when I went carnivore. Murray switched cold turkey and seems to have experienced some unpleasant effects like keto flu, but they resolved after a time.
Summary
- The speaker discovered the carnivore diet through their son, who had successfully lost weight with it.
- The speaker had a history of gout and other health issues, which were not effectively treated by conventional medicine.
- A doctor suggested that diet was the root cause of many diseases, which led the speaker to try the Pritikin diet, resulting in weight loss but not complete gout relief.
- The speaker initially doubted the carnivore diet but was convinced after seeing the positive results on their son and daughter-in-law.
- Adopting the carnivore diet led to significant health improvements, including better mobility, reduced inflammation, and better sleep.
- The speaker experienced a dramatic weight loss, going from 83 kg to 63.7 kg and maintaining a healthy weight around 64-66 kg.
- The diet has resolved various health issues, including irritable bowel syndrome and bleeding bowels.
- The speaker and their wife now follow a lifestyle change, including cooking outdoors and walking more, which has improved their overall well-being.
- The speaker expresses skepticism towards the medical and food industries, believing they contribute to health problems.
- The speaker views the carnivore diet as a miraculous and life-changing switch that has opened up new possibilities for their future health.
So the official place to get it requires a login: https://doi.org/10.1016/S0140-6736(25)01201-2
But the full report can be found on : https://www.donorplatform.org/wp-content/uploads/2025/10/PIIS0140673625012012.pdf
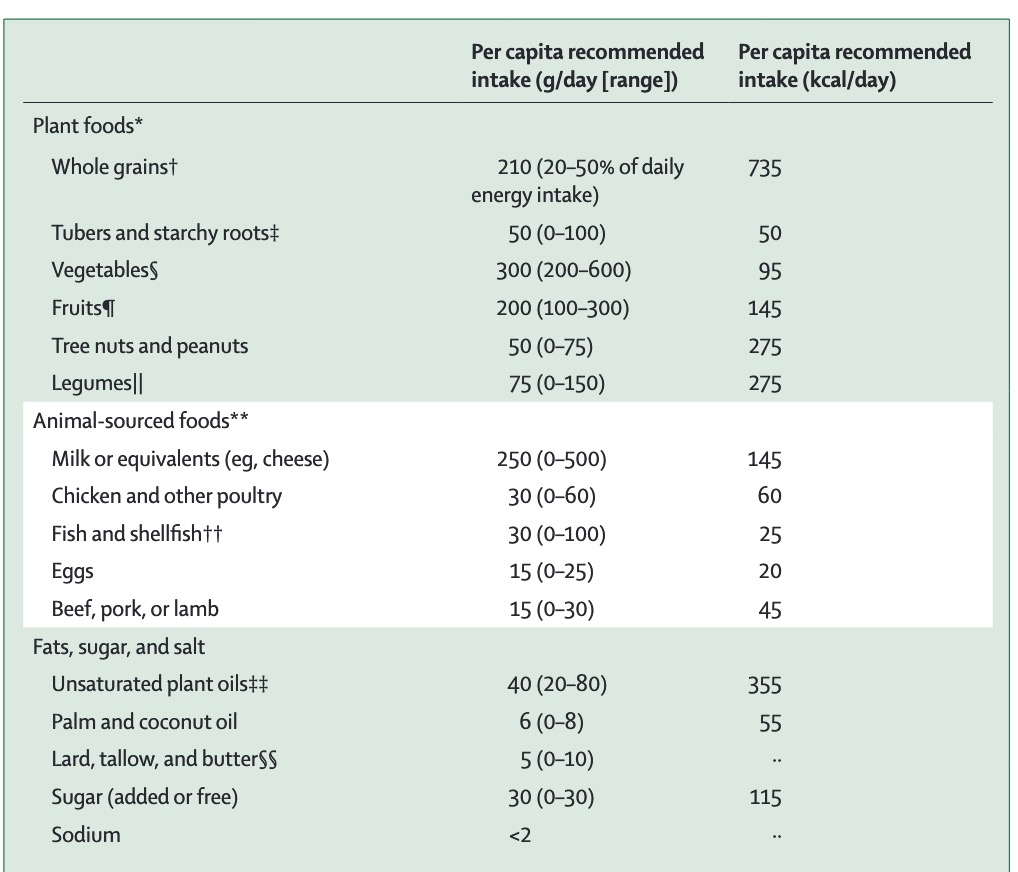
I'll summarize:
60% Carbs, 20% protein, 20% fat
Highly processed seed oils and highly processed grains are the major source of energy on this diet.
Obviously this is counter to the health goals of keto/carnivore, but it's remarkable here as this will be used to drive lots of anti-meat efforts globally, so its good to become familiar with it.
Professor Bart Kay shares his knowledge and experience on carnivore, atherosclerosis, and science.
summerizer
Central Theme
The video repeatedly addresses what the speaker (Bart Kay) describes as an organized “anti-carnivore agenda” — a coordinated effort by mainstream nutrition, pharmaceutical, and media institutions to discredit animal-based diets and protect financial or ideological interests tied to carbohydrate- and seed-oil-based food systems.
Main Claims About the Anti-Carnivore Agenda
1. Economic and Institutional Motives
- Pharmaceutical dependence:
Chronic metabolic illness (type 2 diabetes, obesity, heart disease) sustains lifelong customers for statins, antihypertensives, and insulin-sensitizing drugs.
→ A population reversing these with meat-based diets threatens large pharmaceutical revenue streams. - Agricultural industry alignment:
Plant-based and grain-based commodities are cheaper to produce, store, and market globally.
→ Promoting “heart-healthy grains” and “plant oils” serves corporate agriculture and processed-food sectors. - Academic capture:
Universities and dietetic associations receive funding from cereal, beverage, and pharmaceutical interests, biasing published research and dietary guidelines against saturated-fat and animal-based nutrition.
2. Tactics Used Against the Carnivore / Low-Carb Community
- Media framing and repetition:
- Constantly linking red meat and saturated fat to “heart disease” headlines without mechanistic proof.
- Using relative-risk numbers (e.g., “30 % increase”) that sound alarming but reflect minuscule absolute differences.
- Cherry-picked epidemiology:
- Reliance on weak observational studies with food-frequency questionnaires rather than randomized metabolic trials.
- Ignoring or burying studies showing neutral or beneficial lipid responses in low-carb/carnivore cohorts.
- Terminology control:
- Re-branding seed-oil–based diets as “heart-healthy.”
- Labeling meat-heavy or ketogenic diets as “fad,” “dangerous,” or “unsustainable.”
- Algorithmic suppression:
- Claims that online platforms down-rank or demonetize carnivore content to reduce its visibility while promoting vegan or plant-based material.
- Expert credential attacks:
- Attempts to discredit proponents (Kay, Chaffee, Berry, Baker, etc.) by highlighting lack of dietetic registration or by misrepresenting statements.
- Misuse of LDL narrative:
- LDL is used as a “fear lever” to steer people back to statins and low-fat diets.
- Data challenging LDL causality are said to be ignored or dismissed as “misinformation.”
3. Psychological and Social Levers
- Moral framing:
Associating meat consumption with environmental harm or cruelty to paint carnivore adherents as unethical or regressive. - Fear campaigns:
Continuous repetition of phrases like “artery-clogging saturated fat” to instill subconscious aversion. - Group identity pressure:
Encouraging conformity to plant-based norms via social validation (“everyone knows meat causes heart disease”).
4. Counter-Strategies Proposed
- Educate via mechanistic evidence:
Share physiology showing that insulin resistance, not LDL, drives arterial damage. - Demand primary data and absolute risk figures.
- Avoid debating on moral grounds; focus on metabolic outcomes.
- Build independent research networks and clinical case series demonstrating reversal of metabolic markers on meat-based diets.
- Document personal lab results (fasting insulin, HbA1c, triglyceride-to-HDL ratio) to counter narrative with data.
- Promote transparent funding disclosure in all nutritional research.
- Use decentralized media (podcasts, independent platforms) to bypass censorship and framing bias.
5. Predicted Continuation of the Agenda
- Future policy proposals expected to link climate regulation with “sustainable diets,” thereby legislatively restricting meat production and access.
- The narrative will increasingly merge environmental, ethical, and health justifications to suppress meat consumption across multiple fronts.
Summary Statement
According to the video, the anti-carnivore agenda operates through financial incentives, selective science, and media repetition to preserve existing industrial food and drug profits. The recommended response is radical nutritional self-education, transparent data sharing, and metabolic self-experimentation rather than reliance on institutional dietary authority.
Nina and I talk about women's involvement in the carnivore movement, health risks associated with seed oils, and much more. Make sure to listen to the full interview to learn more.
Nina Teicholz, PhD, is a renowned investigative science journalist and New York Times best-selling author. With a profound commitment to reshaping our understanding of dietary fats, her seminal work, The Big Fat Surprise, challenges decades of conventional wisdom regarding the health impacts of saturated fats and the efficacy of low-fat diets. Teicholz's rigorous investigation reveals the complex interplay of science and politics that has shaped dietary guidelines, urging a reevaluation of nutritional norms that have long been taken for granted.
summerizer
Title: “Is Carnivore a Right-Wing Toxic Masculinity Diet? – Nina Teicholz”
Participants:
- Guest: Nina Teicholz (investigative science journalist; author of The Big Fat Surprise; founder of the Nutrition Coalition)
- Host: Judy Cho, FNTP
Core thesis from the video:
- Media often frames carnivore as a “right-wing/toxic masculinity” fad, but large numbers of women follow the diet and report health-driven reasons and outcomes.
- Conventional nutrition policy and much of nutrition science (especially food-frequency–based epidemiology) are criticized for weak methods, industry influence, and a narrow focus on LDL cholesterol.
- Low-carb/ketogenic patterns—including meat-heavy diets—are presented as legitimate therapeutic options for metabolic disease, while acknowledging gaps (e.g., randomized trials specifically on strict carnivore).
Key points covered:
- Women on carnivore: The conversation centers on Nina’s recent piece highlighting women in the carnivore community and their motivations (symptom relief, metabolic and mental-health improvements, weight, energy, etc.).
- History and context: The video references historical all-meat feeding experiments and early clinical investigations to argue adequacy of animal-sourced diets when well-formulated.
- Evidence the guests cite:
- A Harvard/Boston Children’s survey of >2,000 adults following a carnivore diet reporting high satisfaction and perceived health improvements, with mixed lipid changes and noted LDL-C elevations in a subset. DOI: 10.1093/cdn/nzab133.
- A 2-year, non-randomized clinical trial of a digitally supported ketogenic/lower-carb intervention in type 2 diabetes reporting improvements in HbA1c, weight, triglycerides, blood pressure, inflammatory and liver markers, and reductions in diabetes medications; some lipid changes (including LDL-C) discussed in context. DOI: 10.3389/fendo.2019.00348.
- The host/guest refer to Stanford’s “identical twins” randomized trial comparing vegan vs omnivorous diets (with disclosure about external funding to the research center). The video highlights short-term cardiometabolic shifts and notes concerns around vitamin B12 on vegan patterns. DOI: 10.1001/jamanetworkopen.2023.44457.
- Early 20th-century all-meat feeding work (Bellevue experiment) is mentioned as historical context for adequacy and safety monitoring on meat-only intakes; used to illustrate that meat-exclusive diets have been clinically observed.
- Methodology critiques: The video argues that:
- Food-frequency–questionnaire epidemiology cannot establish causality and is frequently confounded.
- Selective emphasis on LDL-C ignores broader cardiometabolic risk patterns that often improve on carb restriction.
- Funding and institutional incentives shape narratives (e.g., alternative-protein funding in academic centers).
- Policy and guidelines: Nina discusses efforts to improve the scientific rigor and transparency of U.S. Dietary Guidelines processes; she argues the guidelines marginalize low-carb/carnivore-leaning approaches despite clinical signals.
- Media narrative: The guests describe a mismatch between popular/press portrayals of carnivore (political/masculinity framing) and the reported motivations and demographics seen in communities and survey data.
- Research gaps noted in the discussion:
- A lack of randomized controlled trials specifically on strict carnivore.
- Need for longer-term, higher-quality trials tracking hard outcomes and comprehensive nutrient status, especially for women.
Referenced papers with DOIs (as cited/discussed in the video):
- Harvard/Boston Children’s survey of carnivore dieters: 10.1093/cdn/nzab133
- 2-year low-carb/ketogenic T2D intervention (continuous remote care): 10.3389/fendo.2019.00348
- Stanford identical-twin RCT (vegan vs omnivorous, 8 weeks): 10.1001/jamanetworkopen.2023.44457
Tone and takeaway within the video:
- The conversation emphasizes reframing carnivore beyond stereotypes, foregrounding women’s experiences and health motivations, critiquing weak/biased evidence bases, and calling for better, longer-term trials and more open dietary policy processes.
Cary talks about his journey on the carnivore diet.
summerizer
Title: What Happened When I Quietly Tried Carnivore
• Discovery & Motivation
- Learned about carnivore after following low-carb voices (mentions discovering it through a creator named “Butter Bob”).
- Decided to try it quietly without announcing it widely.
• Start & Approach
- Began earlier this year; kept it simple and consistent.
- Focused on meat (especially beef), eggs, and butter; minimized/avoided carbs.
- Typically 1–2 meals per day based on satiety.
• Early Effects
- Rapid changes: clearer thinking, reduced brain fog, noticeable body recomposition.
- Marked drop in hunger and food preoccupation; felt satisfied after meals.
• Ongoing Results
- Continued weight loss and visible leanness (“abs are made in the kitchen” theme).
- Improved overall energy; exercise felt easier (already an active runner).
- Noted insulin control as central to weight and health improvements.
• Daily Eating Details
- Prefers simple, repeatable meals (beef cuts; often mentions chuck eye/ribeye).
- Frequently includes butter; eggs are a staple.
- Eats to satiety, doesn’t force snacks between meals.
• Social & Family Dynamics
- Kept diet mostly private; tells close family because of shared meals.
- Comfortable with others eating differently; cooks separately when needed.
- Brings her own food to social events to stay on track.
• Mindset & Lessons
- Simplicity helps adherence; fewer decisions, less time thinking about food.
- Respect for individual choice: “eat the way that keeps you healthy.”
- Emphasis on consistency over perfection.
Most doctors still treat insulin resistance with medication but what if the real cure starts with food? In this episode, Dr. Eric Westman sits down with Dr. Tony Hampton to reveal how patients are reversing diabetes, dropping A1C from 12 to 6, and regaining their health in just weeks using a simple low-carb food playbook. Backed by CGM data and real clinical results, they expose why medical schools ignore nutrition, how carbs drive insulin spikes, and what foods truly fix metabolism. Whether you're battling blood sugar issues, weight gain, or metabolic syndrome — this conversation will change how you see food forever.
The core message is type 2 diabetes is reversible
summerizer
Title: Fix Insulin Resistance in 2 Weeks?! (Keto Made Simple Podcast with Dr. Eric Westman & Dr. Tony Hampton)
Core message
- Insulin resistance is reversible for most people by removing the drivers: excess carbohydrates/sugar, frequent snacking, poor sleep, chronic stress, and seed-oil–heavy ultra-processed foods.
- Therapeutic carbohydrate restriction (low-carb/keto) can rapidly improve glycemia—often within days—enabling safe, supervised deprescribing of diabetes medications.
Key takeaways
- Dietary strategy
- Remove sugars, refined starches, fruit juices, sweetened drinks, and most grains.
- Center meals on protein (meat, eggs, fish) and add natural fats to satiety; non-starchy vegetables as tolerated.
- Avoid industrial seed oils; choose simpler, minimally processed foods.
- Electrolytes (sodium, potassium, magnesium) may need attention early in keto; hydration matters.
- Expected clinical responses (seen in practice)
- Rapid drops in blood glucose and insulin requirements; some patients reduce or stop insulin very quickly under supervision.
- Improvements in weight, blood pressure, triglycerides/HDL, and markers tied to metabolic syndrome.
- Kidney outcomes discussed: improvement in renal function is reported when glycemia and blood pressure improve.
- Deprescribing approach
- Reduce/stop insulin and sulfonylureas first to avoid hypoglycemia as carbs are lowered.
- Monitor glucose, blood pressure, and symptoms closely; adjust other meds (e.g., antihypertensives) as physiology normalizes.
- Lifestyle frameworks Dr. Hampton uses
- “NEST/ROPE” concepts: Nutrition, Exercise, Stress/Sleep/Trauma foundations (“roots”) that support behavior change; build a trusting relationship first, then implement low-carb.
- Common obstacles & solutions
- Skepticism from clinicians or family; counter with patient results and published evidence.
- Cultural food patterns and access; adapt low-carb within preferred cuisines and local options.
- Long-term success hinges on support, education, and addressing sleep, stress, and environment—not diet alone.
Notes from cases discussed
- Examples of large, rapid insulin reductions when carbohydrate intake is restricted and coaching is provided.
- Emphasis on hope and agency: patients can improve neuropathy risk, vision risk, and amputation risk by treating the root cause (hyperinsulinemia/hyperglycemia).
Papers referenced in the conversation (DOI links)
- Very low-carb/keto vs. DASH randomized trial in adults with hypertension and prediabetes or type 2 diabetes (greater improvements; diabetes remission notably higher in VLCD group).
https://doi.org/10.1370/afm.2968 - Virta Health 1-year outcomes (open-label, non-randomized; substantial A1c reduction, weight loss, and major reductions in diabetes medications including insulin).
https://doi.org/10.1007/s13300-018-0386-4 - Virta Health 2-year outcomes (continued benefits with remote care and nutritional ketosis).
https://doi.org/10.3389/fendo.2019.00348 - Kidney function with low-carb diets in type 2 diabetes (literature review plus 7-year primary-care data; renal function outcomes discussed).
https://doi.org/10.1097/MED.0000000000000658